Imaging case 14:
Breast Cancer - Ductal Carcinoma In Situ
During breast-conserving surgery it is common practice to perform intraoperative assessment of the resected tumor specimen to assess if the resection was successful. This is especially useful for patients diagnosed with Ductal Carcinoma In Situ (DCIS), as the positive margin rate is higher in this population. The most frequently used techniques such as specimen radiography or frozen section assessment all have their drawbacks regarding performance and/or efficiency(1).
In this clinical case, which is part of the multi-center prospective BrIMA study (NCT04999917), we highlight how intraoperative specimen PET-CT imaging can bring more confidence into the operating room. This gives the surgeon a clear view of what was resected – and the ability to act upon this information at the point of surgery.
Patient History
A 66-year old woman with Ductal Carcinoma In-Situ(DCIS) underwent breast-conserving surgery. The tumor size on preoperative imaging was 30mm, biopsy showed a grade 3 tumor, receptor status unknown. Preoperative staging was cTisN0M0.
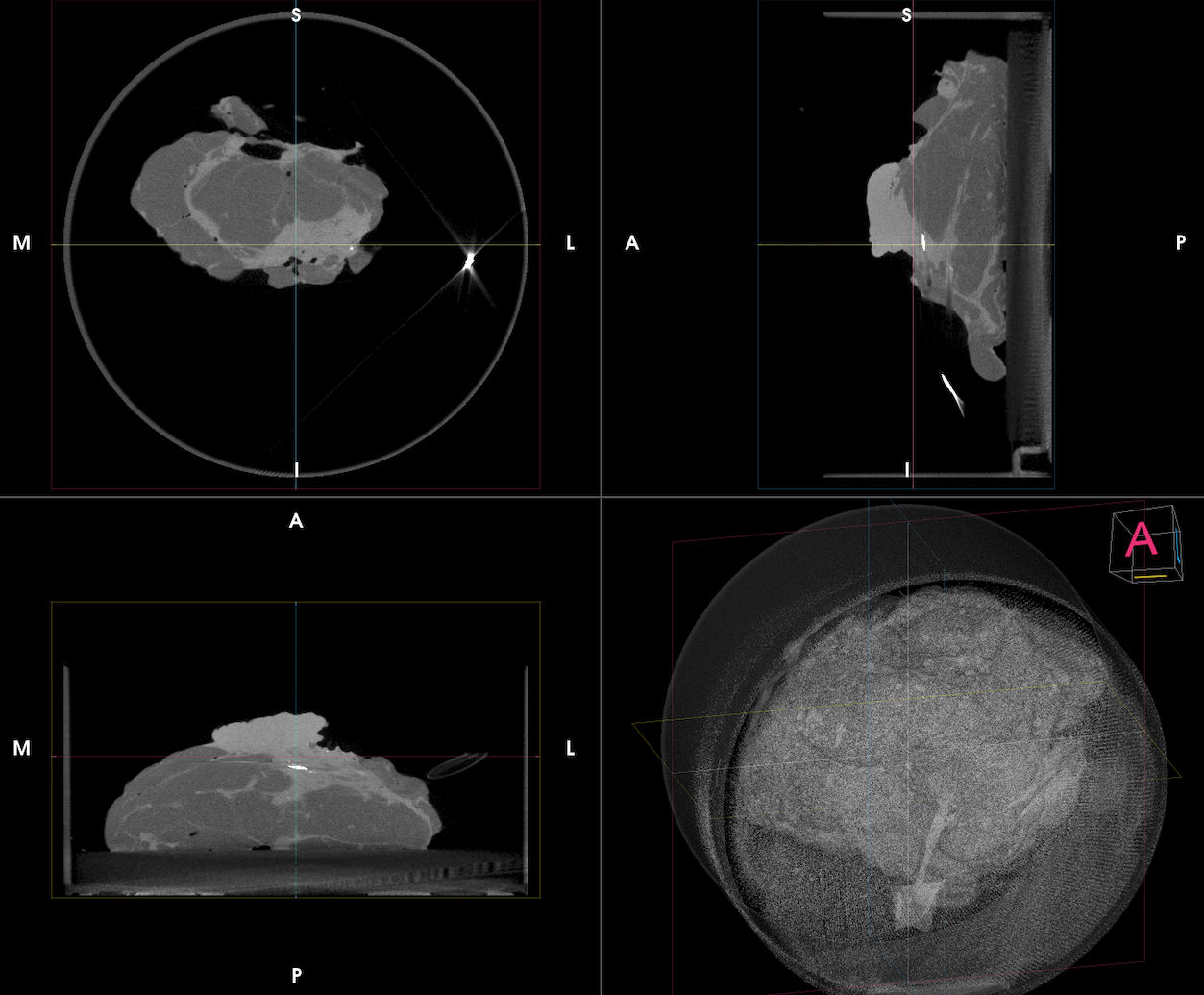 Figure 1. Three orthogonal slices + a 3D render (bottom right) of the CT images of the specimen containing a DCIS lesion. A dense lump is visualized in the inferior region of the specimen.
Figure 1. Three orthogonal slices + a 3D render (bottom right) of the CT images of the specimen containing a DCIS lesion. A dense lump is visualized in the inferior region of the specimen.
PET-CT specimen images
An intravenous injection with 70 MBq (0.80 MBq/Kg) of 18F-FDG was given on the morning of the surgery at the Nuclear Medicine Department. The patient was then transferred to the operating theatre and breast-conserving surgery was performed per standard protocol. Based on standard-of-care per-op specimen radiography it was estimated that the entire lesion was resected, so no oriented cavity shaving was recommended based on this assessment.
The resected breast specimen was imaged with the XEOS AURA 10 imager immediately afterwards and the images were interpreted by the surgeon in the operating room. This was approximately 103 min after 18F-FDG injection. The CT (Fig. 1) visualizes the entire specimen in 3D and an area of dense tissue was visible in the inferior region of the specimen. This already provides an indication of where the tumor is located in the specimen. Microcalcifications can be observed due to the high spatial resolution (100µm) of the CT image.
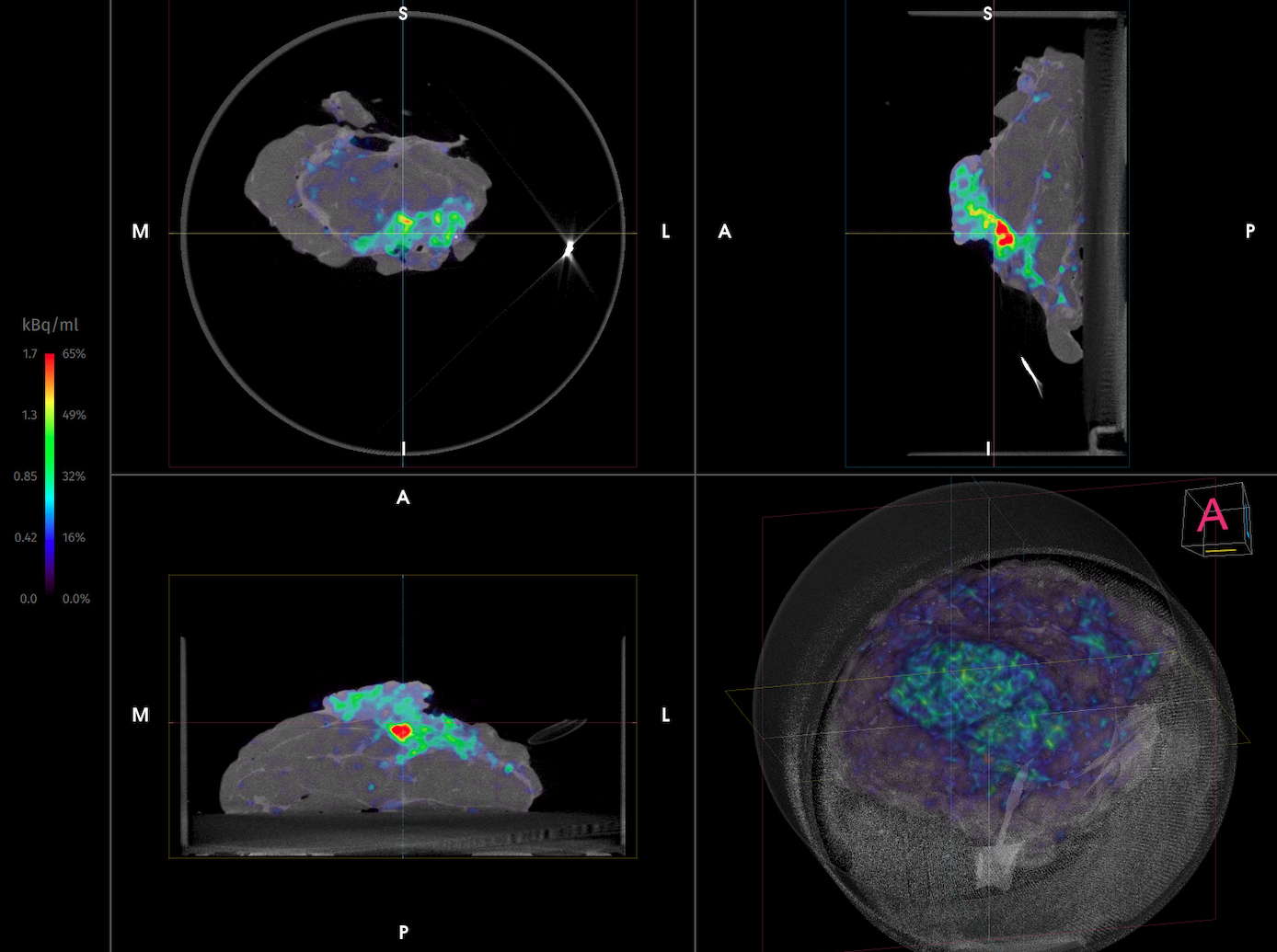
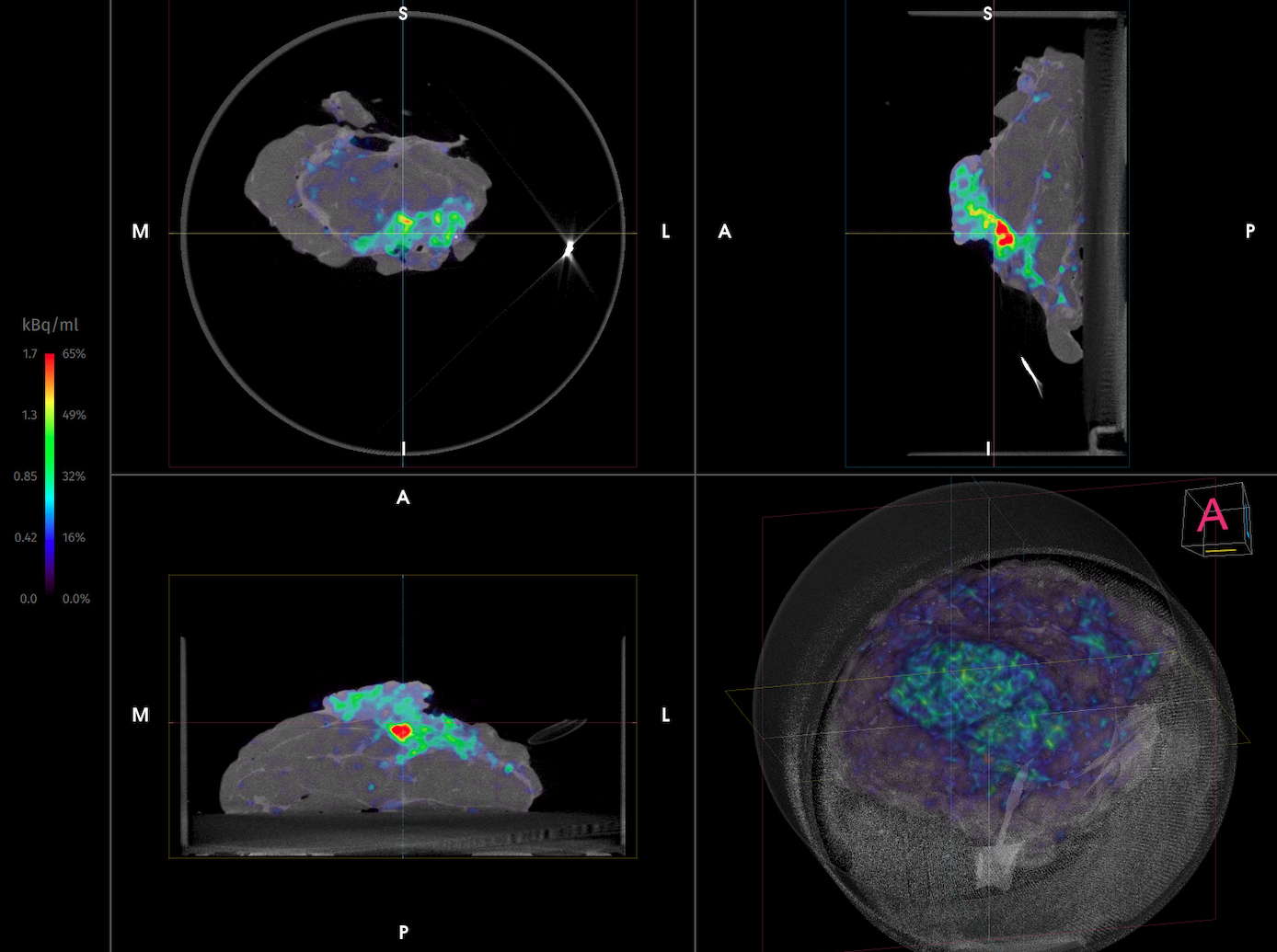 Figure 2. Three orthogonal slices + a 3D render (bottom right) of the PET-CT images of the specimen containing a DCIS lesion showing increased 18F-FDG uptake at the inferior border. Postoperative final pathology showed that there was only a tumor-free margin of <1mm at the inferior side.
Figure 2. Three orthogonal slices + a 3D render (bottom right) of the PET-CT images of the specimen containing a DCIS lesion showing increased 18F-FDG uptake at the inferior border. Postoperative final pathology showed that there was only a tumor-free margin of <1mm at the inferior side.
Fig. 2 shows the per-op specimen PET-CT images, highlighting increased 18F-FDG uptake at the inferior border, which indicates metabolically more active regions such as cancer cells. Based on this image, the surgeon decided to take a cavity shave in this area.
Histopathological Evaluation
Immediately after specimen imaging, the resected specimen was sent to the pathology department for routine histopathological evaluation, which was available after several days. Table 1 shows the results of histopathology. Postoperative final pathology showed that there was only a tumor-free margin of <1mm at the inferior side, where 2mm tumor-free margin is required in BCS for DCIS.
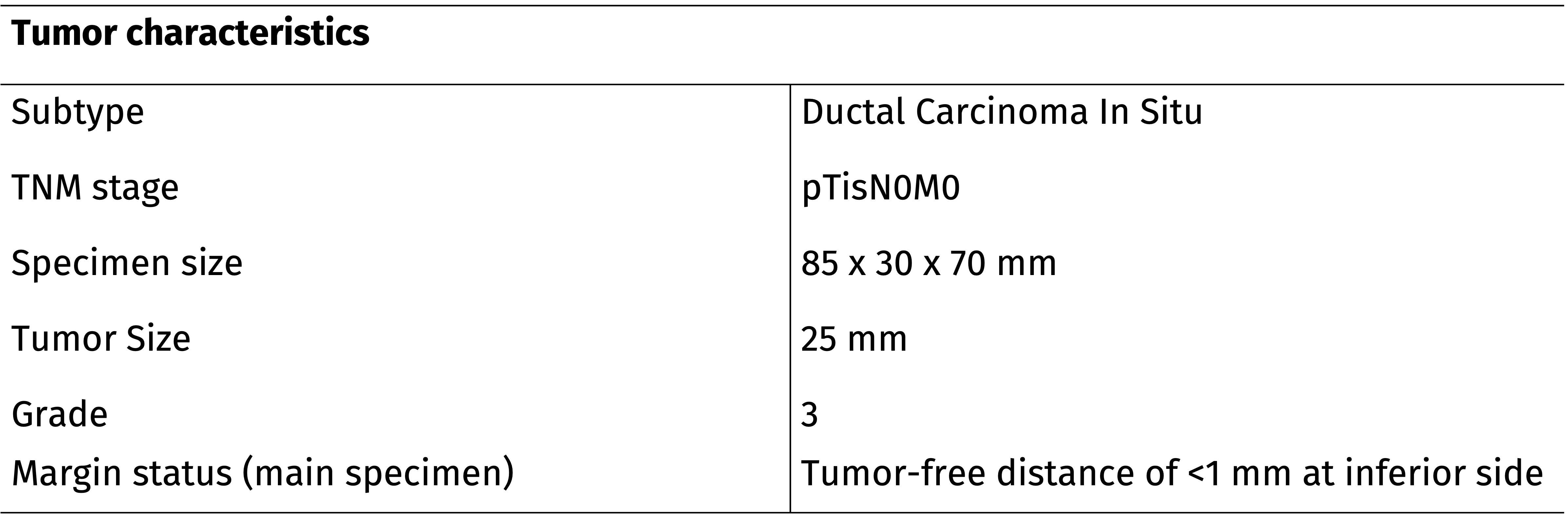 Table 1. A summary of the histopathological findings of the resected specimens.
Table 1. A summary of the histopathological findings of the resected specimens.
Discussion and Conclusion
In this interesting case, the surgeon decided to perform an additional cavity shave based on specimen PET-CT imaging as 18F-FDG uptake was reaching the inferior border of the specimen. Histopathological evaluation also showed only a tumor-free margin of <1 mm was reached at the inferior border. In this patient the additional cavity shave helped to avoid the need for reoperation and the associated burden.
REFERENCES
[1] St John et al, Diagnostic Accuracy of Intraoperative Techniques for Margin Assessment in Breast Cancer Surgery: A Meta-analysis. Ann Surg 2017.