Imaging case 23:
Head & Neck cancer - Squamous Cell carcinoma of the retromolar trigone
When treating patients for oral squamous cell carcinoma surgeons aim to obtain marginal clearance by at least 5 mm. Due to the complicated three-dimensional anatomy, it can be difficult to be certain that all resection margins are clear when treating oral squamous cell carcinoma in locations such as the retromolar or palatal area. Close or involved margins may require re-excision or more frequently adjuvant radiotherapy treatment which leads to additional morbidity for patients - some of the effects of which are life-long. Additionally, close or involved margins result in a higher risk of treatment failure particularly if a bone margin is involved as adjuvant treatment is less effective in bone compared to soft tissue.
This case highlights how intraoperative specimen PET-CT imaging can give the surgeon a clear view of the extent of the tumor in the resected specimen and therefore give the surgeon confidence and the ability to act upon this information at the point of surgery.
The case is presented with the support of Mr. Gary Walton, consultant head and neck surgeon, Dr. Oludolapo Adesanya, consultant radiologist, and colleagues of University Hospitals Coventry & Warwickshire, Coventry, United Kingdom, as part of the ‘eXcision’ trial (IRAS ID: 342171, REC reference 24/YH/0137). The ‘eXcision’ trial is a single center prospective pilot study investigating the diagnostic performance of high-resolution specimen PET-CT imaging in prostate cancer and head and neck cancer resection.
Patient History
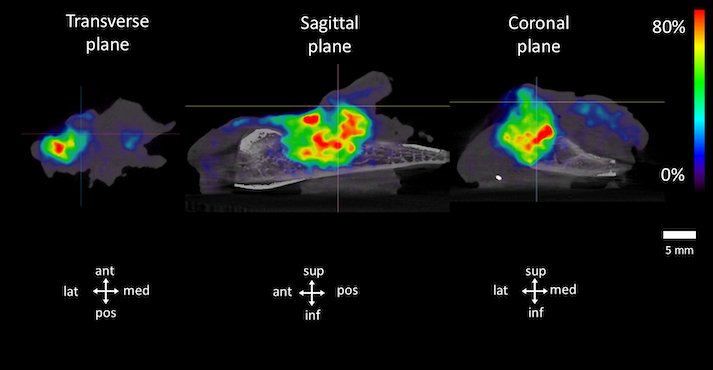
A 65-year-old patient was diagnosed with a right sided retromolar tumor. Preoperative staging with MRI and CT imaging yielded inconclusive findings regarding bone invasion. The patient was scheduled for resection of the tumor, i.e., a right hemi-mandibulectomy with a right neck dissection and free flap reconstruction.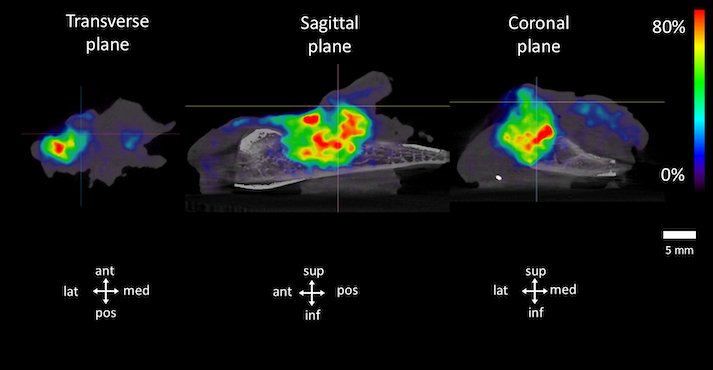 Figure 1. Transverse, coronal, and sagittal slices of the PET-CT specimen images of the resected tumor specimen. A 3D image is shown as well. Specimen orientation is as indicated. Abbreviations: med, medial; lat, lateral; sup, superior; inf, inferior; ant, anterior; pos, posterior. A window of 0-80% was used for representing radiotracer uptake.
Figure 1. Transverse, coronal, and sagittal slices of the PET-CT specimen images of the resected tumor specimen. A 3D image is shown as well. Specimen orientation is as indicated. Abbreviations: med, medial; lat, lateral; sup, superior; inf, inferior; ant, anterior; pos, posterior. A window of 0-80% was used for representing radiotracer uptake.
Specimen PET-CT images
The patient was injected with 40 MBq of 18F-FDG at the start of the surgery.
Resection of the primary tumor was completed at approximately 120 min after injection. Immediately after resection, a high-resolution specimen PET-CT image was acquired in the operating theatre with the XEOS AURA 10 PET-CT imager. The images are shown in Fig. 1.
 Figure 2. Specimen PET-CT image of the resected tumor specimen, for different planes with 18F-FDG uptake close to the lateral region, the posterior submucosal region, medial mucosal region, and deep region, respectively. A window of 0-80% was used for representing radiotracer uptake. Orientation of the specimen is indicated on the figure.
Figure 2. Specimen PET-CT image of the resected tumor specimen, for different planes with 18F-FDG uptake close to the lateral region, the posterior submucosal region, medial mucosal region, and deep region, respectively. A window of 0-80% was used for representing radiotracer uptake. Orientation of the specimen is indicated on the figure.
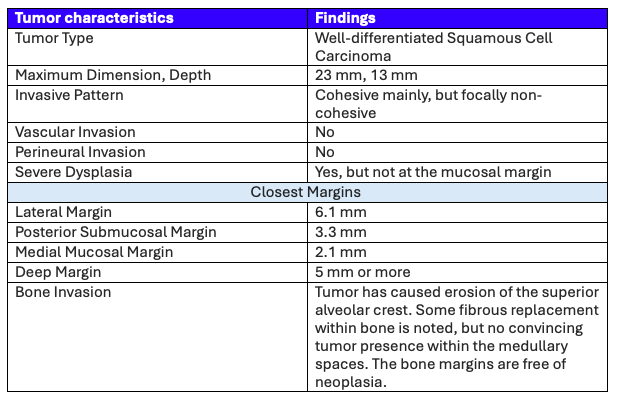 Table 1: A summary of the histopathological findings of the resected specimens.
Table 1: A summary of the histopathological findings of the resected specimens.
Histopathological Evaluation
After PET-CT imaging, the surgical specimen was sent to the pathology department for routine histopathological evaluation. This evaluation was available after more than two weeks. Table 1 shows the results of histopathology.
The regions exhibiting radiotracer uptake near the specimen's border corresponded to the anatomical regions where the closest margins were seen on histopathology. All clinically relevant margins are wider than 5 mm and hence sufficient for oncological safety. The only close margins (< 5 mm) are the medial mucosal and posterior submucosal margin, both oriented towards the oral cavity and therefore do not imply an indication for immediate adjuvant therapy. Histopathological evaluation also confirmed bone invasion as suspected on specimen PET-CT imaging.
Given the depth of the bone invasion, the staging was set at NM8 – PT3 - R0.
Discussion and conclusion
Radiotracer uptake near the specimen's border was observed in anatomical regions corresponding to the closest margins identified on histopathology. The only margins measuring less than 5 mm are directed toward the oral cavity, and thus, do not warrant immediate adjuvant therapy. Importantly, pathology usually takes a minimum of fourteen days, and even longer if bone invasion needs to be confirmed. Therefore, this case underscores the potential usefulness of specimen PET-CT imaging for head and neck cancer. It could provide critical information at the point of surgery and so could help surgeons to assess completeness of resection and may reduce the need for adjuvant therapy in selected patients.References
Debacker JM et al. High-Resolution 18F-FDG PET/CT for Assessing Three-Dimensional Intraoperative Margins Status in Malignancies of the Head and Neck, a Proof-of-Concept. J Clin Med 2021; 10:3737.